Controlling Periodontal Disease
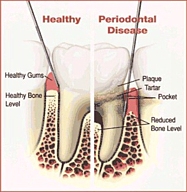
Maintaining good oral health goes beyond brushing teeth a couple of times a day, daily flossing and the use of a good mouthwash. Even by being scrupulous with at home hygiene, over time, bio film (plaque) will adhere to teeth and harden. The plaque will form in hard to reach areas, creating pockets where bacteria can grow, requiring a professional cleaning. It is the excess accumulation of bacteria that causes the local periodontal tissue to become inflamed (gingivitis). If left untreated, gingivitis will progress to a more chronic condition, periodontitis (periodontal disease). When inflammation is present, oral bacteria and its byproducts, called endotoxins, can enter the general blood circulation. It is the body’s secondary inflammatory response to these circulating bacteria that is implicated in the complication of many medical conditions and diseases. The goal of periodontal treatment is to remove inflammation-causing bacteria from the mouth, thereby preserving tooth health and decreasing overall systemic inflammation.
Behavioral and biological risk factors also play a role in the progression of periodontal disease. These include:
Smoking or chewing tobacco
Stress Family history of periodontal disease
Ill fitting fillings, crooked teeth, food impaction areas
Medications
Other systemic diseases
Depending on the severity of the periodontal disease, the treatment will vary. For mild disease, scaling and root planing is recommended, along with creating new oral hygiene habits to eliminate its recurrence. It is important to follow through with the follow-up evaluation to confirm the status of your oral health. If the disease is more moderate, then scaling and root planing and improved oral hygiene habits may be accompanied by the administration of local and/or systemic antibiotics, as well as more frequent scheduled hygiene appointments to help manage the disease. If this is not sufficient, surgical intervention may be necessary to remove diseased tissue, eliminate pocket depth or regenerate lost supporting tissue. When periodontal disease is advanced, treatment options may change again. In addition to the treatment recommendations of moderate periodontal disease, more aggressive periodontal surgery and/or tooth removal may be necessary.
Your Next Steps
Your next step will be to have a Periodontal Risk Evaluation by a periodontist or dentist who is highly qualified to diagnose and treat periodontal disease. During your evaluation, your medical history will be carefully reviewed. Your blood pressure will be noted. Full mouth x-rays will be examined for radiographic signs of periodontal disease destruction. Most importantly, each tooth will be evaluated for:
Attachment loss
Bleeding upon probing
Pocket depth
Recession
The presence of pus
Mobility
Occlusion (bite relationship)
Adequacy of existing restorations
These results will be noted on a periodontal chart. This information, along with the other factors will lead to a specific diagnosis of periodontal disease. If periodontal inflammatory disease is present, a course of recommended treatment will be established. Additionally, the prognosis and recommendations for maintenance will be established. The results of your Periodontal Risk Evaluation will be sent to your physician(s) to become part of your medical record.